- Y Diweddaraf sydd Ar Gael (Diwygiedig)
- Pwynt Penodol mewn Amser (18/12/2009)
- Gwreiddiol (Fel y’i mabwysiadwyd gan yr UE)
Council Directive of 26 June 1964 on animal health problems affecting intra-Community trade in bovine animals and swine (64/432/EEC)
You are here:
- Cyfarwyddebau yn deillio o’r UE
- 1964 No. 432
- Annexes only
- Dangos Graddfa Ddaearyddol(e.e. Lloegr, Cymru, Yr Alban aca Gogledd Iwerddon)
- Dangos Llinell Amser Newidiadau
Rhagor o Adnoddau
PDF o Fersiynau Diwygiedig
- ddiwygiedig 27/05/20151.04 MB
- ddiwygiedig 01/01/20151.08 MB
- ddiwygiedig 17/07/20141.20 MB
- ddiwygiedig 01/07/20131.20 MB
- ddiwygiedig 18/12/20091.20 MB
- ddiwygiedig 31/12/20080.43 MB
- ddiwygiedig 03/09/20080.43 MB
- ddiwygiedig 13/11/20070.45 MB
- ddiwygiedig 05/01/20070.45 MB
- ddiwygiedig 09/07/20050.58 MB
- ddiwygiedig 01/05/20040.57 MB
- ddiwygiedig 29/07/20020.59 MB
- ddiwygiedig 12/04/20020.58 MB
- ddiwygiedig 31/07/20010.60 MB
- ddiwygiedig 04/07/20000.68 MB
- ddiwygiedig 03/05/20002.86 MB
- ddiwygiedig 31/12/19980.46 MB
- ddiwygiedig 15/07/19980.46 MB
- ddiwygiedig 01/07/19980.25 MB
- ddiwygiedig 30/06/19640.46 MB
Pan adawodd y DU yr UE, cyhoeddodd legislation.gov.uk ddeddfwriaeth yr UE a gyhoeddwyd gan yr UE hyd at ddiwrnod cwblhau’r cyfnod gweithredu (31 Rhagfyr 2020 11.00 p.m.). Ar legislation.gov.uk, mae'r eitemau hyn o ddeddfwriaeth yn cael eu diweddaru'n gyson ag unrhyw ddiwygiadau a wnaed gan y DU ers hynny.
Mae'r eitem hon o ddeddfwriaeth yn tarddu o'r UE
Mae legislation.gov.uk yn cyhoeddi fersiwn y DU. Mae EUR-Lex yn cyhoeddi fersiwn yr UE. Mae Archif Gwe Ymadael â’r UE yn rhoi cipolwg ar fersiwn EUR-Lex o ddiwrnod cwblhau’r cyfnod gweithredu (31 Rhagfyr 2020 11.00 p.m.).
Changes over time for: Council Directive of 26 June 1964 on animal health problems affecting intra-Community trade in bovine animals and swine (64/432/EEC) (Annexes only)
Version Superseded: 01/01/2015
Alternative versions:
- 09/07/2005- Amendment
- 05/01/2007- Amendment
- 13/11/2007- Amendment
- 03/09/2008- Amendment
- 31/12/2008- Amendment
- 18/12/2009- Amendment
- 18/12/2009
Point in time - 01/01/2015- Amendment
- 27/05/2015- Amendment
- Exit day: start of implementation period31/01/2020 11pm- Amendment
- End of implementation period31/12/2020- Amendment
Status:
Cyhoeddir Cyfarwyddebau’r UE ar y wefan hon i gynorthwyo croesgyfeirio o ddeddfwriaeth y DU. Ers diwrnod cwblhau’r cyfnod gweithredu (31 Rhagfyr 2020 11.00 p.m.) nid oes unrhyw ddiwygiadau wedi'u cymhwyso i'r fersiwn hon.
[F1 [F2ANNEX A U.K.
Textual Amendments
I. Officially tuberculosis-free bovine herd U.K.
For the purposes of this section ‘ bovine animals ’ means all bovine animals with the exception of animals taking part in cultural or sporting events.
1. A bovine herd is officially tuberculosis-free if: U.K.
all the animals are free from clinical signs of tuberculosis;
all the bovine animals over six weeks old have reacted negatively to at least two official intradermal tuberculin tests carried out in accordance with Annex B, the first six months after the elimination of any infection from the herd and the second six months later or, where the herd has been assembled solely from animals that originate in officially tuberculosis-free herds, the first test shall be carried out at least 60 days after assembly and the second shall not be required;
following the completion of the first test referred to in (b), no bovine animal over six weeks old has been introduced into the herd unless it has reacted negatively to an intradermal tuberculin test performed and assessed according to Annex B and carried out either in the 30 days prior to, or the 30 days after the date of its introduction into the herd; in the latter case the animal(s) must be isolated physically from the other animals of the herd in a way to avoid any direct or indirect contact with the other animals until proven negative.
However, the competent authority may not require this test to be carried out for movements of animals on its own territory if the animal is from an officially tuberculosis-free herd, except in a Member State where, on 1 January 1998 and until the status of officially tuberculosis-free region is obtained, the competent authority required such tests to be carried out for animals moving between herds participating in a network system as referred to in Article 14.
2. A bovine herd will retain officially tuberculosis-free status if: U.K.
the conditions detailed in 1(a) and (c) continue to apply;
all animals entering the holding come from herds of officially tuberculosis-free status;
all animals on the holding, with the exception of calves under six weeks old which were born in the holding, are subjected to routine tuberculin testing in accordance with Annex B at yearly intervals.
However, the competent authority of a Member State may, for the Member State or part of the Member State where all the bovine herds are subject to an official programme to combat tuberculosis, alter the frequency of the routine tests as follows:
if the average — determined at 31 December of each year — of the annual percentages of bovine herds confirmed as infected with tuberculosis is not more than 1 % of all herds within the defined area during the two most recent annual supervisory periods, the interval between routine herd tests may be increased to two years and male animals for fattening within an isolated epidemiological unit may be exempted from tuberculin testing provided that they come from officially tuberculosis-free herds and that the competent authority guarantees that the males for fattening will not be used for breeding and will go direct for slaughter,
if the average — determined at 31 December of each year — of the annual percentages of bovine herds confirmed as infected with tuberculosis is not more than 0,2 % of all herds within the defined area during the two most recent biennial supervisory periods, the interval between routine tests may be increased to three years and/or the age at which animals have to undergo these tests may be increased to 24 months,
if the average — determined at 31 December of each year — of the annual percentages of bovine herds confirmed as infected with tuberculosis is not more than 0,1 % of all herds within the defined area during the two most recent supervisory triennial periods, the interval between routine tests may be increased to four years, or, providing the following conditions are met, the competent authority may dispense with tuberculin testing of the herds:
(1)before the introduction into the herd all the bovine animals are subjected to an intradermal tuberculin test with negative results;
[F3or]
(2)all bovine animals slaughtered are examined for lesions of tuberculosis and any such lesions are submitted to a histopathological and bacteriological examination for evidence of tuberculosis.
The competent authority may also, in respect of the Member State or a part thereof, increase the frequency of tuberculin testing if the level of the disease has increased.
Textual Amendments
3A. The officially tuberculosis-free status of a herd is to be suspended if: U.K.
the conditions detailed in paragraph 2 are no longer fulfilled;
or
one or more animals are deemed to have given a positive reaction to a tuberculin test, or a case of tuberculosis is suspected at post-mortem examination.
When an animal is considered to be a positive reactor it will be removed from the herd and slaughtered. Appropriate post-mortem, laboratory and epidemiological examinations shall be carried out on the positive reactor or the carcase of the suspect animal. The status of the herd will remain suspended until such time as all laboratory examinations have been completed. If the presence of tuberculosis is not confirmed, the suspension of the officially tuberculosis-free status may be lifted following a test of all animals over six weeks of age with negative results at least 42 days after the removal of the reactor animal(s);
or
the herd contains animals of unresolved status as described in Annex B. In this case, the status of the herd is to remain suspended until the animals' status has been clarified. Such animals must be isolated from the other animals of the herd until their status has been clarified, either by a further test after 42 days or by post-mortem and laboratory examination;
however, by way of derogation from the requirements of paragraph (c), in a Member State where the competent authority carries out routine herd testing using the comparative tuberculin test described in Annex B, and in the case of a herd where no confirmed reactor animals have been disclosed for at least three years, the competent authority may decide not to restrict the movement of other animals in the herd, provided that the status of any inconclusive reactors is resolved by a further test after 42 days and that no animals from the holding are allowed to enter into intra-Community trade until the status of any inconclusive reactors has been resolved. If at this further test any animal either gives a positive reaction or continues to give an inconclusive reaction, then the conditions of paragraph (b) apply. If the presence of disease is subsequently confirmed, all animals leaving the holding since the time of the last clear herd test must be traced and tested.
3B. The officially tuberculosis-free status of the herd is to be withdrawn if the presence of tuberculosis is confirmed by the isolation of M. bovis on laboratory examination. U.K.
The competent authority may withdraw status if:
the conditions detailed in point 2 are no longer fulfilled, or
classical lesions of tuberculosis are seen at post-mortem examination, or
an epidemiological enquiry establishes the likelihood of infection,
or for any other reasons considered necessary for the purpose of controlling bovine tuberculosis.
Tracing and checking is to be undertaken by the competent authority of any herd considered to be epidemiologically related. The officially tuberculosis-free status of a herd is to remain withdrawn until cleansing and disinfection of the premises and utensils has been completed and all animals over six weeks of age have reacted negatively to at least two consecutive tuberculin tests, the first no less than 60 days and the second no less than four months and no more than 12 months after the removal of the last positive reactor.
4. On the basis of information supplied in accordance with Article 8, a Member State or part of a Member State may be declared officially tuberculosis-free according to the procedure laid down in Article 17 if it meets the following conditions: U.K.
the percentage of bovine herds confirmed as infected with tuberculosis has not exceeded 0,1 % per year of all herds for six consecutive years and at least 99,9 % of herds have achieved officially tuberculosis-free status each year for six consecutive years, the calculation of this latter percentage to take place on 31 December each calendar year;
[F4each bovine animal is identified in accordance with Community legislation, and]
all bovine animals slaughtered are subjected to an official post-mortem examination;
the procedures for suspension and withdrawal of officially tuberculosis-free status are complied with.
Textual Amendments
5. The Member State or part of a Member State will retain officially tuberculosis-free status if the conditions 4(a) to (d) continue to be met. However, if there is evidence of a significant change in the situation as regards tuberculosis in a Member State or part of a Member State which has been recognised as officially tuberculosis-free, the Commission may, in accordance with the procedure laid down in Article 17, take a Decision suspending or revoking the status until the requirements of the Decision have been fulfilled. U.K.
II. Officially brucellosis-free and brucellosis-free bovine herds U.K.
For the purposes of this section ‘ bovine animals ’ means all bovine animals with the exception of males for fattening provided that they come from officially brucellosis-free herds and that the competent authority guarantees that the males for fattening will not be used for breeding and will go direct for slaughter.
1. A bovine herd is officially brucellosis-free if: U.K.
it contains no bovine animals which have been vaccinated against brucellosis, except females which have been vaccinated at least three years previously;
all the bovine animals have been free from clinical signs of brucellosis for at least six months;
all the bovine animals over 12 months old have been subjected to one of the following test regimes with negative results in accordance with Annex C:
two serological tests specified in paragraph 10 at an interval of more than three months and less than 12 months;
three tests on milk samples at three-monthly intervals followed at least six weeks later by a serological test specified in paragraph 10;
any bovine animal entering the herd comes from a herd of officially brucellosis-free status and, in the case of bovine animals over 12 months old, has shown a brucella titre of less than 30 IU of agglutination per ml when given a serum agglutination test in accordance with Annex C or has reacted negatively to any other test approved in accordance with the procedure at Article 17 during the 30 days prior to or the 30 days after the date of its introduction into the herd: in the latter case, the animal(s) must be isolated physically from the other animals of the herd in such a way as to avoid direct or indirect contact with the other animals until proven negative.
2. A bovine herd will retain officially brucellosis-free status if: U.K.
one of the following test regimes is carried out annually with negative results in accordance with Annex C:
three milk ring tests carried out at intervals of at least three months;
three milk ELISAs carried out at intervals of at least three months;
two milk ring tests carried out at an interval of at least three months followed at least six weeks later by a serological test referred to in paragraph 10;
two milk ELISAs carried out at an interval of at least three months followed at least six weeks later by a serological test referred to in paragraph 10;
two serological tests carried out at an interval of at least three months and not more than 12 months.
However, the competent authority of a Member State may, for the Member State or part of the Member State which is not officially brucellosis-free but where all the bovine herds are subject to an official programme to combat brucellosis, alter the frequency of the routine tests as follows:
where not more than 1 % of bovine herds are infected, it may be sufficient to carry out each year two milk ring tests or two milk ELISAs at an interval of at least three months, or one serological test,
where at least 99,8 % of bovine herds have been recognised as officially brucellosis-free for at least four years, the interval between checks may be extended to two years if all animals over 12 months of age are tested, or testing may be restricted to animals over 24 months of age if herds continue to be tested each year. The checks must be carried out using one of the serological tests referred to in paragraph 10;
all bovine animals entering the herd come from herds of officially brucellosis-free status and, in the case of bovine animals over 12 months old, have shown a brucella titre of less than 30 IU of agglutination per ml when given a serum agglutination test in accordance with Annex C or have reacted negatively to any other test approved in accordance with the procedure at Article 17 during the 30 days prior to or the 30 days after the date of their introduction into the herd; in the latter case, the animal(s) must be isolated physically from the other animals of the herd in such a way as to avoid direct or indirect contact with the other animals until proven negative.
However, the test described in point (b) need not be required in Member States, or regions of Member States, where the percentage of bovine herds infected with brucellosis has not exceeded 0,2 % for at least two years and where the animal comes from an officially brucellosis-free bovine herd within that Member State or region and has not during transportation come into contact with bovine animals of lesser status;
notwithstanding point (b), bovine animals from a brucellosis-free bovine herd may be introduced into an officially brucellosis-free herd if they are at least 18 months old and, if vaccinated against brucellosis, the vaccination was carried out more than a year previously.
Such animals must have shown, in the 30 days prior to introduction, a brucella titre lower than 30 IU of agglutination per ml and a negative result when given a complement fixation test, or other test approved under the procedure set out in Article 17.
If, however, a female bovine animal from a brucellosis-free herd is introduced into an officially brucellosis-free herd, under the provisions of the above paragraph, that herd shall be considered to be brucellosis-free for two years from the date on which the last vaccinated animal was introduced.
3A. The officially brucellosis-free status of a herd is to be suspended if: U.K.
the conditions detailed in paragraphs 1 and 2 are no longer fulfilled; or
as a result of laboratory tests or on clinical grounds one or more bovine animals is suspected of having brucellosis and the suspect animals have been slaughtered or isolated in a way to avoid any direct or indirect contact with the other animals.
Where the animal has been slaughtered and is no longer available for testing, the suspension may be lifted if two serum agglutination tests, carried out in accordance with Annex C on all bovine animals in the herd over 12 months old, show a titre lower than 30 IU of agglutination per ml. The first test shall be carried out at least 30 days after the removal of the animal and the second at least 60 days later.
Where the animal has been isolated from the animals in the herd, it may be reintroduced into the herd and the status of the herd may be restored following:
a serum agglutination test which has shown a titre lower than 30 IU of agglutination per ml and has given a negative result to a complement fixation test, or
a negative result to any other combination of tests approved for that purpose under the procedure set out in Article 17.
3B. The officially brucellosis-free status of the herd is to be withdrawn if, as a result of laboratory tests or epidemiological investigations, brucella infection has been confirmed in the herd. U.K.
The status of the herd is not to be restored until either all bovine animals present in the herd at the time of the outbreak have been slaughtered, or the herd has been subject to check testing and all animals over 12 months of age have given negative results to two consecutive tests at 60-day intervals, the first being carried out not less than 30 days after removal of the positive animal(s).
In the case of bovine animals which were pregnant at the time of the outbreak, the final check must be carried out at least 21 days after the last animal pregnant at the time of the outbreak has calved.
4. A bovine herd is brucellosis-free if it complies with the conditions in 1(b) and (c) and when vaccination has been carried out as follows: U.K.
female bovine animals have been vaccinated:
before the age of six months old with live strain 19 vaccine, or
before the age of 15 months old with killed 45/20 adjuvant vaccine which has been officially inspected and approved, or
with other vaccines approved under the procedure laid down in Article 17;
bovine animals under 30 months old which have been vaccinated with live strain 19 vaccine may give a serum agglutination test result greater than 30 IU but less than 80 IU of agglutination per millilitre provided that, on the complement fixation test, they give a result less than 30 EEC units in the case of females vaccinated less than 12 months previously or less than 20 EEC units in all other cases.
5. A bovine herd will retain brucellosis-free status if: U.K.
it is subject to one of the testing regimes listed in 2(a);
bovine animals entering the herd comply with the requirements of 2(b); or
come from herds of brucellosis-free status, and in the case of bovine animals over 12 months old, have shown, in the 30 days prior to or in isolation after introduction into the herd, less than 30 IU of agglutination per ml when given a serum agglutination test and a negative result to a complement fixation test in accordance with Annex C, or
come from herds of brucellosis-free status, are under 30 months old and have been vaccinated with live strain 19 vaccine if they give a serum agglutination test result greater than 30 IU but less than 80 IU of agglutination per millilitre provided that, on the complement fixation test, they give a result less than 30 EEC units in the case of females vaccinated less than 12 months previously or less than 20 EEC units in all other cases.
6A. The brucellosis-free status of a herd is to be suspended if: U.K.
the conditions detailed in paragraphs 4 and 5 have not been complied with; or
as a result of laboratory tests or on clinical grounds one or more bovine animals over 30 months old is suspected of having brucellosis and the animal(s) under suspicion have been slaughtered, or isolated in a way to avoid any direct or indirect contact with other animals.
Where the animal has been isolated, it may be reintroduced into the herd and the status of the herd may be restored, if it subsequently shows a serum agglutination titre lower than 30 IU of agglutination per ml and has given a negative result to a complement fixation test, or other test approved under the procedure set out in Article 17.
Where the animals have been slaughtered and are no longer available for testing, the suspension may be lifted if two serum agglutination tests, carried out in accordance with Annex C on all bovine animals in the holding over 12 months old, show a titre lower than 30 IU of agglutination per ml. The first test is to be carried out at least 30 days after the removal of the animal and the second at least 60 days later.
If the animals to be tested in the previous two subparagraphs are under 30 months old and have been vaccinated with live strain 19 vaccine they may be considered to be negative if they give a serum agglutination test result greater than 30 IU but less than 80 IU of agglutination per millilitre provided that, on the complement fixation test, they give a result less than 30 EEC units in the case of females vaccinated less than 12 months previously or less than 20 EEC units in all other cases.
6B. The brucellosis-free status of the herd is to be withdrawn if, as a result of laboratory tests of epidemiological investigations, brucella infection has been confirmed in a herd. The status of the herd is not to be restored until either all the bovine animals present in the herd at the time of the outbreak have been slaughtered or the herd has been subject to check testing and all unvaccinated animals over 12 months of age have given negative results to two consecutive tests at 60 day intervals, the first being carried out not less than 30 days after removal of the positive animal(s). U.K.
If all the animals to be tested referred to in the preceding paragraph are less than 30 months old and have been vaccinated with live strain 19 vaccine, they may be considered negative if they show a brucella titre of more than 30 IU but less than 80 IU of agglutination per ml, provided that in the complement fixation test they show a titre of less than 30 EEC units in the case of females vaccinated less than 12 months previously or a titre of less than 20 EEC units in all other cases.
In the case of bovine animals which were pregnant at the time of the outbreak, the final check must have been carried out at least 21 days after the last animal pregnant at the time of the outbreak has calved.
7. A Member State or a region of a Member State may be declared officially brucellosis-free according to the procedure laid down in Article 17 if it meets the following conditions: U.K.
no case of abortion due to brucella infection and no isolation of B. abortus has been recorded for at least three years and at least 99,8 % of herds have achieved officially brucellosis-free status each year for five consecutive years, the calculation of this percentage to take place on 31 December each calendar year. However, where the competent authority adopts a policy of whole herd slaughter, isolated incidents shown by epidemiological enquiry to be due to the introduction of animals from outside the Member State or part of the Member State and herds whose officially brucellosis-free status has been suspended or withdrawn for reasons other than suspicion of disease, is to be disregarded for the purpose of the above calculation provided that the central competent authority of the Member State concerned by these incidents makes an annual record and forwards them to the Commission in accordance with Article 8(2), and
[F4each bovine animal is identified in accordance with Community legislation, and]
notification of cases of abortion is mandatory and they are investigated by the competent authority.
8. Subject to paragraph 9, a Member State or a region of a Member State declared officially brucellosis-free is to retain this status if: U.K.
the conditions imposed by paragraph 7(a) and (b) are still fulfilled and notification of cases of abortion suspected of being due to brucellosis is mandatory and are investigated by the competent authority;
every year for the first five years after attaining status, all bovine animals over 24 months of age in not less than 20 % of herds have been tested and have reacted negatively to a serological test carried out in accordance with Annex C or, in the case of dairy herds, by examination of milk samples in accordance with Annex C;
every bovine animal suspected of being infected with brucellosis is notified to the competent authority and undergoes official epidemiological investigation for brucellosis comprising at least two serological blood tests, including the complement fixation test, and a microbiological examination of appropriate samples;
during the period of suspicion, which is to continue until negative results have been obtained from the tests provided for in (c), the officially brucellosis-free status of the herd of origin or transit of the suspected bovine animal and of the herds linked epidemiologically to it is to be suspended;
in the event of an outbreak of brucellosis that has spread, all bovine animals have been slaughtered. Animals of the remaining susceptible species will undergo appropriate tests and premises and equipment will be cleaned and disinfected.
9. A Member State or a region of a Member State declared officially brucellosis-free is to report the occurrence of all cases of brucellosis to the Commission. If there is evidence of a significant change in the situation as regards brucellosis in a Member State or part of a Member State which has been recognised as officially brucellosis-free, the Commission may according to the procedure laid down in Article 17 propose that the status be suspended or revoked until the requirements of the Decision have been fulfilled. U.K.
10. For the purposes of section II, a serological test means either a serum agglutination test, buffered brucella antigen test, complement fixation test, plasma agglutination test, plasma ring test, micro-agglutination test or individual blood ELISA, as described in Annex C. Any other diagnostic test approved under the procedure laid down in Article 17 and described in Annex C will also be accepted for the purposes of section II. A milk test means a milk ring test or a milk ELISA in accordance with Annex C.] U.K.
[F5ANNEX B U.K. TUBERCULOSIS
Textual Amendments
1. IDENTIFICATION OF THE AGENT U.K.
The presence of Mycobacterium bovis (M. bovis) , agent of bovine tuberculosis, in clinical and post-mortem specimens may be demonstrated by examination of stained smears or immunoperoxidase techniques and confirmed by cultivation of the organism on primary isolation medium.
Pathological material for the confirmation of M. bovis should be taken from abnormal lymph nodes and parenchymatous organs such as lungs, liver, spleen, etc. In the cases where the animal does not present pathological lesions, samples from the retropharyngeal, bronchial, mediastinal, supramammary, mandibular and some mesenteric lymph nodes and liver should be collected for examination and culture.
Identification of isolates may be usually carried out by determining cultural and biochemical properties. The polymerase chain reaction (PCR) may also be employed for the detection of the M. tuberculosis complex. DNA analysis techniques may prove to be faster and more reliable than biochemical methods for the differentiation of M. bovis from other members of the M. tuberculosis complex. Genetic fingerprinting allows distinguishing between different strains of M. bovis and will enable patterns of origin, transmission and spread of M. bovis to be described.
The techniques and media used, their standardisation and the interpretation of results must conform to that specified in the OIE Manual of Standards for Diagnostic Tests and Vaccines, Fourth Edition, 2000, Chapter 2.3.3 (bovine tuberculosis).
2. THE TUBERCULIN SKIN TEST U.K.
Tuberculin PPD (Purified Protein Derivatives) that fulfil the standards laid down in paragraph 2.1 shall be used for carrying out official tuberculin skin test following the procedures referred to in paragraph 2.2.
2.1. Standards for tuberculin (bovine and avian) U.K.
2.1.1. Definition U.K.
Tuberculin purified protein derivative (tuberculin PPD, bovine or avian) is a preparation obtained from the heat-treated products of growth and lysis of Mycobacterium bovis or Mycobacterium avium (as appropiate) capable of revealing a delayed hypersensitivity in an animal sensitised to microorganisms of the same species.
2.1.2. Production U.K.
It is obtained from the water-soluble fractions prepared by heating in free-flowing steam and subsequently filtering cultures of M. bovis or M. avium (as appropiate) grown in a liquid synthetic medium. The active fraction of the filtrate, consisting mainly of protein, is isolated by precipitation, washed and re-dissolved. An antimicrobial preservative that does not give rise to false positive reactions, such as phenol, may be added. The final sterile preparation, free from mycobacteria, is distributed aseptically into sterile tamper-proof glass containers which are then closed so as to prevent contamination. The preparation may be freeze-dried.
2.1.3. Identification of the product U.K.
Inject a range of graded doses intradermally at different sites into suitably sensitised albino guinea-pigs, each weighing not less than 250 g. After 24 h to 28 h, reactions appear in the form of oedematous swellings with erythema with or without necrosis at the points of injection. The size and severity of the reactions vary according to the dose. Unsensitised guinea-pigs show no reactions to similar injections.
2.1.4. Tests U.K.
2.1.4.1. pH: The pH is 6.5 to 7.5. U.K.
2.1.4.2. Phenol: If the preparation to be examined contains phenol, its concentration is not more than 5 g/l. U.K.
2.1.4.3. Sensitising effect: Use a group of three guinea-pigs that have not been treated with any material which will interfere with the test. On 3 occasions at intervals of five days inject intradermally into each guinea-pig a dose of the preparation to be examined equivalent to 500 IU in 0,1 ml. 15 to 21 days after the third injection inject the same dose (500 IU) intradermally into these animals and into a control group of three guinea-pigs of the same mass and which have not previously received injections of tuberculin. 24 to 28 hours after the last injections, the reactions of the two groups are not significantly different. U.K.
2.1.4.4. Toxicity: Use two guinea-pigs, each weighing not less than 250 g and which have not previously been treated with any material which will interfere with the test. Inject subcutaneously into each guinea-pig 0,5 ml of the preparation to be examined. Observe the animals for seven days. No abnormal effects occur during the observation period. U.K.
2.1.4.5. Sterility: It complies with the test for sterility prescribed in the monograph on Vaccines for veterinary use 4th Edition 2002 of the European Pharmacopoeia. U.K.
2.1.5. Potency U.K.
The potency of tuberculin purified protein derivative (bovine and avian) is determined by comparing the reactions produced in sensitised guinea-pigs by the intradermal injection of a series of dilutions of the preparation to be examined with those produced by known concentrations of a reference preparation of tuberculin (bovine or avian, as appropiate) purified protein derivative calibrated in International Units.
To test the potency, sensitise not fewer than nine albino guinea-pigs, each weighing 400 g to 600 g, by the deep intramuscular injection of 0,0001 mg of wet mass of living M. bovis of strain AN5 suspended in 0.5 ml of a 9 g/l solution of sodium chloride R for bovine tuberculin, or a suitable dose of inactivated or live M. avium for avian tuberculin. Not less than four weeks after the sensitisation of the guinea-pigs, shave their flanks to provide space for not more than four injection sites on each side. Prepare dilutions of the preparation to be examined and of the reference preparation using isotonic phosphate-buffered saline (pH 6,5-7,5) containing 0,005 g/l of polysorbate 80 R. Use not fewer than three doses of the reference preparation and not fewer than three doses of the preparation to be examined. Choose the doses such that the lesions produced have a diameter of not less than 8 mm and not more than 25 mm. Allocate the dilutions randomly to the sites using a Latin square design. Inject each dose intradermally in a constant volume of 0,1 ml or 0,2 ml. Measure the diameters of the lesions after 24 to 28 hours and calculate the result of the test using the usual statistical methods and assuming that the diameters of the lesions are directly proportional to the logarithm of the concentration of the tuberculins.
The test is not valid unless the fiducial limits of error (P = 0,95) are not less than 50 % and not more then 200 % of the estimated potency. The estimated potency is not less than 66 % and not more than 150 % of the stated potency for bovine tuberculin. The estimated potency is not less than 75 % and not more than 133 % of the stated potency for avian tuberculin. The stated potency is not less than 20 000 IU/ml for both tuberculins (bovine and avian).
2.1.6. Storage U.K.
Store protected from light, at a temperature of 5 ± 3 o C.
2.1.7. Labelling U.K.
The label states:
the potency in International Units per millilitre,
the name and quantity of any added substance,
for freeze-dried preparations:
-the name and volume of the reconstituting liquid to be added,
-that the product should be used immediately after reconstitution.
2.2. Test procedures U.K.
2.2.1. The following shall be recognised as official intradermal tuberculin tests: U.K.
the single intradermal test: this test requires a single injection of bovine tuberculin,
the intradermal comparative test: this test requires one injection of bovine tuberculin and one injection of avian tuberculin given simultaneously.
2.2.2. The dose of tuberculin injected shall be: U.K.
not less than 2 000 IU of bovine tuberculin,
not less than 2 000 IU of avian tuberculin.
2.2.3. The volume of each injection dose shall not exceed 0,2 ml. U.K.
2.2.4. Tuberculin tests shall be carried out by injecting tuberculin(s) into the skin of the neck. The injection sites shall be situated at the border of the anterior and middle thirds of the neck. When both avian and bovine tuberculins are injected in the same animal, the site for injection of avian tuberculins shall be about 10 cm from the crest of the neck and the site for the injection of bovine tuberculin about 12,5 cm lower on a line roughly parallel with the line of the shoulder or on different sides of the neck; in young animals in which there is not room to separate the sites sufficiently on one side of the neck, one injection shall be made on each side of the neck at identical sites in the centre of the middle third of the neck. U.K.
2.2.5. The technique of tuberculin testing and interpretation of reactions shall be as follows: U.K.
2.2.5.1. Technique: U.K.
Injection sites shall be clipped and cleansed. A fold of skin within each clipped area shall be taken between the forefinger and thumb and measured with callipers and recorded. The dose of tuberculin shall then be injected by a method that ensures that the tuberculin is delivered intradermically. A short sterile needle, bevel edge outwards, with graduated syringe charged with tuberculin, inserted obliquely into the deeper layers of the skin may be used. A correct injection shall be confirmed by palpating a small pea-like swelling at each site of injection. The skin-fold thickness of each injection site shall be remeasured 72 hours (± 4 hours) after injection and recorded.
2.2.5.2. Interpretation of reactions U.K.
The interpretation of reactions shall be based on clinical observations and the recorded increase(s) in skin-fold thickness at the sites of injection 72 hours after injection of tuberculin(s).
Negative reaction: if only limited swelling is observed, with an increase of not more than 2 mm in the thickness of the fold of skin without clinical signs such as diffuse or extensive oedema, exudation, necrosis, pain or inflammation of the lymphatic ducts in that region or of the lymph nodes.
Inconclusive reaction: if no clinical signs such as mentioned in a) are observed and if the increase in skin-fold thickness is more than 2 mm and less than 4 mm.
Positive reaction: if clinical signs such as mentioned in a) are observed or there is an increase of 4 mm or more in the thickness of the fold of skin at the injection site.
2.2.5.3. The interpretation of official intradermal tuberculin tests shall be as follows: U.K.
2.2.5.3.1. Single intradermal test: U.K.
positive: a positive bovine reaction as defined in paragraph 2.2.5.2(c);
inconclusive: an inconclusive reaction as defined in paragraph 2.2.5.2(b);
negative: a negative bovine reaction as defined in paragraph 2.2.5.2(a).
Animals inconclusive to the single intradermal test shall be subjected to another test after a minimum of 42 days.
Animals which are not negative to this second test shall be deemed to be positive to the test.
Animals positive to the single intradermal test may be subjected to an intradermal comparative test if false positive reaction or interference reaction is suspected.
2.2.5.3.2. Intradermal comparative test for the establishment and maintenance of officially tuberculosis-free herd status: U.K.
positive: a positive bovine reaction which is more than 4 mm greater than the avian reaction, or the presence of clinical signs;
inconclusive: a positive or inconclusive bovine reaction which is from 1 to 4 mm greater than the avian reaction, and the absence of clinical signs;
negative: a negative bovine reaction, or a positive or inconclusive bovine reaction but which is equal to or less than a positive or inconclusive avian reaction and the absence of clinical signs in both cases.
Animals inconclusive to the intradermal comparative test shall be subjected to another test after a minimum of 42 days. Animals, which are not negative to this second test, shall be deemed to be positive to the test.
2.2.5.3.3. Officially tuberculosis-free herd status may be suspended and animals from the herd shall not be allowed to enter intra-Community trade until such time as the status of the following animals is resolved: U.K.
animals which have been deemed to be inconclusive to the single intradermal tuberculin test;
animals which have been deemed to be positive to the single intradermal tuberculin test but are awaiting retest with an intradermal comparative test;
animals which have been deemed to be inconclusive to the intradermal comparative test.
2.2.5.3.4. Where animals are required by Community legislation to be subjected to an intradermal test prior to movement, the test shall be interpreted so that no animal which shows an increase in skin-fold thickness greater than 2 mm or the presence of clinical signs is entered into intra-Community trade. U.K.
2.2.5.3.5. To enable detection of the maximum number of infected and diseased animals in a herd or in a region, Member States may modify the criteria for the interpretation of the test in order to achieve improved test sensitivity considering all inconclusive reactions referred in 2.2.5.3.1(b) and 2.2.5.3.2(b) as positive reactions. U.K.
3. SUPPLEMENTARY TESTING U.K.
To enable detection of the maximum number of infected and diseased animals in a herd or in a region, Member States may authorise the employ of the gamma-interferon assay referred in the OIE Manual of Standards for Diagnostic Tests and Vaccines, 4th Edition, 2000, Chapter 2.3.3. (bovine tuberculosis), in addition to the tuberculin test.
4. STATE INSTITUTES AND NATIONAL REFERENCE LABORATORIES U.K.
[F64.1. Tasks and responsibilities U.K.
The State institutes, national reference laboratories or official institutes designated in accordance with Article 6a shall be responsible for the official testing of tuberculins or reagents referred to in paragraphs 2 and 3 respectively in their respective Member States to ensure that each of these tuberculins or reagents is adequate in relation to the standards referred to in point 2.1 and paragraph 3 respectively.] ]
Textual Amendments
F6 Substituted by Council Directive 2008/73/EC of 15 July 2008 simplifying procedures of listing and publishing information in the veterinary and zootechnical fields and amending Directives 64/432/EEC, 77/504/EEC, 88/407/EEC, 88/661/EEC, 89/361/EEC, 89/556/EEC, 90/426/EEC, 90/427/EEC, 90/428/EEC, 90/429/EEC, 90/539/EEC, 91/68/EEC, 91/496/EEC, 92/35/EEC, 92/65/EEC, 92/66/EEC, 92/119/EEC, 94/28/EC, 2000/75/EC, Decision 2000/258/EC and Directives 2001/89/EC, 2002/60/EC and 2005/94/EC (Text with EEA relevance).
F7. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .U.K.
[F8 [F9ANNEX C U.K. BRUCELLOSIS
Textual Amendments
1. IDENTIFICATION OF THE AGENT U.K.
The demonstration by modified acid-fast or immunospecific staining of organisms of Brucella morphology in abortion material, vaginal discharges or milk provides presumptive evidence of brucellosis, especially if supported by serological tests. The polymerase chain reaction (PCR) methods provide additional means of detection.
Whenever possible, Brucella spp. should be isolated using plain or selective media by culture from uterine discharges, aborted foetuses, udder secretions or selected tissues, such as lymph nodes and male and female reproductive organs.
After isolation, the species and biovar shall be identified by phage lysis and/or oxidative metabolism tests, cultural, biochemical and serological criteria. PCR can provide both a complementary and biotyping method based on specific genomic sequences.
The techniques and media used, their standardisation and the interpretation of results must conform to that specified in the OIE Manual of Diagnostic Tests and Vaccines for Terrestrial Animals, Sixth Edition, 2008, Chapter 2.4.3 (bovine brucellosis), Chapter 2.7.2 (caprine and ovine brucellosis) and Chapter 2.8.5 (porcine brucellosis).
2. IMMUNOLOGICAL TESTS U.K.
2.1. Standards U.K.
2.1.1. The Brucella abortus biovar 1 Weybridge strain No 99 or USDA strain 1119-3 must be used for the preparation of all antigens used in the rose Bengal test (RBT), serum agglutination test (SAT), complement fixation test (CFT) and the milk ring test (MRT). U.K.
2.1.2. The standard reference serum for the RBT, SAT, CFT and MRT shall be the OIE international reference standard serum (OIEISS) formerly named WHO second international anti- Brucella abortus Serum (ISAbS). U.K.
2.1.3. The standard reference sera for enzyme-linked immunosorbent assays (ELISAs) shall be: U.K.
the OIEISS,
the weak positive OIE ELISA standard serum (OIEELISA WP SS),
the strong positive OIE ELISA standard serum (OIEELISA SP SS),
the negative OIE ELISA standard serum (OIEELISA N SS).
2.1.4. The standard reference sera for fluorescence polarisation assays (FPAs) shall be: U.K.
the weak positive OIE ELISA standard serum (OIEELISA WP SS),
the strong positive OIE ELISA standard serum (OIEELISA SP SS),
the negative OIE ELISA standard serum (OIEELISA N SS).
2.1.5. The standard sera listed in 2.1.3 and 2.1.4 are available from the Community reference laboratory for brucellosis or the Veterinary Laboratories Agency (VLA), Weybridge, United Kingdom. U.K.
2.1.6. The OIEISS, the OIEELISA WP SS, the OIEELISA SP SS and the OIEELISA N SS are international primary standards from which secondary reference national standards serum (working standards) must be established for each test referred to in 2.1.1 in each Member State. U.K.
2.2. Enzyme-linked immunosorbent assays (ELISAs) or other binding assays for the detection of bovine brucellosis in serum or milk U.K.
2.2.1. Material and reagents U.K.
The technique used and the interpretation of results must have been validated in accordance with the principles laid down in Chapter 1.1.4 of the OIE Manual of Diagnostic Tests and Vaccines for Terrestrial Animals, Sixth Edition, 2008, and must include at least laboratory and diagnostic studies.
2.2.2. Standardisation of the test U.K.
2.2.2.1. Standardisation of the test procedure for individual serum samples: U.K.
a 1/150 pre-dilution (1) of the OIEISS or a 1/2 pre-dilution of the OIEELISA WP SS or a 1/16 pre-dilution of the OIEELISA SP SS made up in a negative serum (or in a negative pool of sera) must give a positive reaction;
a 1/600 pre-dilution of the OIEISS or a 1/8 pre-dilution of the OIEELISA WP SS or a 1/64 pre-dilution of the OIEELISA SP SS made up in a negative serum (or in a negative pool of sera) must give a negative reaction;
the OIEELISA N SS must always give a negative reaction.
2.2.2.2. Standardisation of the test procedure for pooled serum samples: U.K.
a 1/150 pre-dilution of the OIEISS or a 1/2 pre-dilution of the OIEELISA WP SS or a 1/16 pre-dilution of the OIEELISA SP SS made up in a negative serum (or in a negative pool of sera) and again diluted in negative sera by the number of samples making up the pool must give a positive reaction;
the OIEELISA N SS must always give a negative reaction;
the test must be adequate to detect evidence of infection in a single animal of the group of animals, of which samples of serum have been pooled.
2.2.2.3. Standardisation of the test procedure for pooled milk or whey samples: U.K.
a 1/ 1 000 pre-dilution of the OIEISS or a 1/16 pre-dilution of the OIEELISA WP SS or a 1/125 pre-dilution of the OIEELISA SP SS made up in a negative serum (or in a negative pool of sera) and again diluted 1/10 in negative milk must give a positive reaction;
the OIEELISA N SS diluted 1/10 in negative milk must always give a negative reaction;
the test must be adequate to detect evidence of infection in a single animal of the group of animals, of which samples of milk or whey have been pooled.
2.2.3. Conditions for use of the ELISAs for diagnosis of bovine brucellosis: U.K.
2.2.3.1. Using the calibrating conditions for ELISAs set out in point 2.2.2.1 and 2.2.2.2 on serum samples, the diagnostic sensitivity of ELISA shall be equal or greater than the RBT or CFT taking into account the epidemiological situation under which it is employed. U.K.
2.2.3.2. Using the calibrating conditions for ELISA set out in point 2.2.2.3 on pooled milk samples, the diagnostic sensitivity of ELISA shall be equal or greater than the MRT taking into account not only the epidemiological situation but also the average and expected extreme husbandry systems. U.K.
2.2.3.3. Where ELISAs are used for certification purposes in accordance with Article 6(1) or for the establishment and maintenance of a herd status in accordance with Annex A(II)(10), pooling of samples of serum must be carried out in such a way that the test results can be undoubtedly related to the individual animal included in the pool. Any confirmatory test must be carried out on samples of serum taken from individual animals. U.K.
2.2.3.4. The ELISAs may be used on a sample of milk taken from the milk collected from a farm with at least 30 % of dairy cows in milk. If that method is used, measures must be taken to ensure that the samples taken for examination can be undoubtedly related to the individual animals from which the milk derived. Any confirmatory test must be carried out on samples of serum taken from individual animals. U.K.
2.3. Complement fixation test (CFT) U.K.
2.3.1. The antigen represents a bacterial suspension in phenol-saline (NaCl 0,85 % (m/v) and phenol at 0,5 % (v/v)) or in a veronal buffer. Antigens may be delivered in the concentrated state provided the dilution factor to be used is indicated on the bottle label. The antigen must be stored at 4 °C and not frozen. U.K.
2.3.2. Serums must be inactivated as follows: U.K.
bovine serum: 56 to 60 °C for 30 to 50 minutes,
porcine serum: 60 °C for 30 to 50 minutes.
2.3.3. In order to carry out the genuine reaction within the test procedure, a complement dose higher than the minimum necessary for total haemolysis shall be used. U.K.
2.3.4. In carrying out the complement fixation test, the following controls must be made each time: U.K.
control of the anti-complementary effect of the serum;
control of the antigen;
control of sensitised red blood cells;
control of the complement;
control using a positive serum of sensitivity at the start of the reaction;
control of the specificity of the reaction using a negative serum.
2.3.5. Calculation of results U.K.
The OIEISS contains 1 000 international CFT units (ICFTU) per ml. If the OIEISS is tested in a given method the result is given as a titre (i.e. highest direct dilution of the OIEISS giving 50 % haemolysis, T OIEISS ). The test result for the test serum given as titre (T TESTSERUM ) must be expressed in ICFTU per ml. In order to convert the expression of a titre into ICFTU, the factor (F) necessary to convert a titre of an unknown test serum (T TESTSERUM ) tested by that method into the ICFTU expression can be found from the formula:
F = 1 000 × 1/T OIEISS
and the content of international CFT units per ml of test serum (ICFTU TESTSERUM ) from the formula:
ICFTU TESTSERUM = F × T TESTSERUM
2.3.6. Interpretation of results U.K.
A serum containing 20 or more ICFTU per ml shall be considered to be positive.
2.4. Milk ring test (MRT) U.K.
2.4.1. The antigen represents a bacterial suspension in phenol-saline (NaCl 0,85 % (m/v) and phenol at 0,5 % (v/v)) stained with haematoxylin. The antigen must be stored at 4 °C and not frozen. U.K.
2.4.2. The antigen sensitivity must be standardised in relation to the OIEISS in such a way that the antigen produces a positive reaction with a 1/500 dilution of the OIEISS in negative milk, while a 1/ 1 000 dilution must be negative. U.K.
2.4.3. The ring test must be made on samples representing the contents of each milk churn or the content of each bulk tank from the farm. U.K.
2.4.4. The milk samples must not have been frozen, heated or subjected to violent shaking. U.K.
2.4.5. The reaction must be carried out using one of the following methods: U.K.
on a column of milk of at least 25 mm height and on a volume of milk of 1 ml to which either 0,03 ml or 0,05 ml of one of the standardised stained antigens has been added,
on a column of milk of at least 25 mm height and on a volume of milk of 2 ml to which 0,05 ml of one of the standardised stained antigens has been added,
on a volume of milk of 8 ml to which 0,08 ml of one of the standardised stained antigens has been added.
2.4.6. The mixture of milk and antigens must be incubated at 37 °C for 60 minutes, together with positive and negative working standards. A subsequent 16- to 24-hours incubation at 4 °C increases the sensitivity of the test. U.K.
2.4.7. Interpretation of results: U.K.
negative reaction: coloured milk, colourless cream;
positive reaction:
identically coloured milk and cream, or
colourless milk and coloured cream.
2.5. Buffered Brucella antigen test (Rose Bengal test (RBT)) U.K.
2.5.1. The antigen represents a bacterial suspension in buffered Brucella antigen diluent at a pH of 3,65 ± 0,05, stained by the use of rose Bengal dye. The antigen shall be delivered ready for use and must be stored at 4 °C and not frozen. U.K.
2.5.2. The antigen shall be prepared without reference to the cell concentration, but its sensitivity must be standardised in relation to the OIEISS in such a way that the antigen produces a positive reaction with a serum dilution of 1/45 and a negative reaction with a dilution of 1/55. U.K.
2.5.3. The RBT shall be carried out in the following manner: U.K.
serum (20-30 μl) is mixed with an equal volume of antigen on a white tile or enamel plate to produce a zone approximately 2 cm in diameter. The mixture is rocked gently for four minutes at ambient temperature, and then observed in a good light for agglutination;
an automated method may be used but must be at least as sensitive and accurate as the manual method.
2.5.4. Interpretation of results U.K.
Any visible reaction shall be considered to be positive, unless there has been excessive drying round the edges.
Positive and negative working standards shall be included in each series of tests.
2.6. Serum agglutination test (SAT) U.K.
2.6.1. The antigen represents a bacterial suspension in phenol-saline (NaCl 0,85 % (m/v) and phenol at 0,5 % (v/v)). U.K.
Formaldehyde must not be used.
Antigens may be delivered in the concentrated state provided the dilution factor to be used is indicated on the bottle label.
EDTA may be added to the antigen suspension to 5 mM final test dilution to reduce the level of false positives to the serum agglutination test. Subsequently the pH of 7.2 must be readjusted in the antigen suspension.
2.6.2. The OIEISS contains 1 000 international units of agglutination. U.K.
2.6.3. The antigen shall be prepared without reference to the cell concentration, but its sensitivity must be standardised in relation to the OIEISS in such a way that the antigen produces either a 50 % agglutination with a final serum dilution of 1/600 to 1/ 1 000 or 75 % agglutination with a final serum dilution of 1/500 to 1/750. U.K.
It may also be advisable to compare the reactivity of new and previously standardised batches of antigen using a panel of defined sera.
2.6.4. The test shall be performed either in tubes or in microplates. The mixture of antigen and serum dilutions shall be incubated for 16- to 24-hours at 37 °C. U.K.
At least three dilutions must be prepared for each serum. Dilutions of suspect serum must be made in such a way that reading of the reaction at the positivity limit is made in the median tube (or well for the microplate method).
2.6.5. Interpretation of results: U.K.
The degree of Brucella agglutination in a serum must be expressed in IU per ml.
A serum containing 30 or more IU per ml is considered to be positive.
2.7. Fluorescence polarisation assay (FPA) U.K.
2.7.1. The FPA can be performed in glass tubes or a 96-well plate format. The technique used, its standardisation and the interpretation of results must conform to that specified Chapter 2.4.3 (bovine brucellosis) of the OIE Manual of Diagnostic Tests and Vaccines for Terrestrial Animals, Sixth Edition, 2008. U.K.
2.7.2. Standardisation of the test U.K.
The FPA shall be standardised so that:
the OIEELISA SP SS and OIEELISA WP SS consistently give positive results.
a 1/8 pre-dilution of the OIEELISA WP SS or a 1/64 pre-dilution of the OIEELISA SP SS made up in a negative serum (or in a negative pool of sera) always gives a negative reaction;
the OIEELISA N SS always gives a negative reaction.
The following shall be included in each batch of tests: a strong positive, a weak positive, a negative working standard serum (calibrated against the OIE ELISA Standard Sera).
3. COMPLEMENTARY TESTS U.K.
3.1. Brucellosis skin test (BST) U.K.
3.1.1. Conditions for the use of BST U.K.
(a) The brucellosis skin test shall not be used for the purpose of certification for intra-Community trade. U.K.
(b) The brucellosis skin test is one of the most specific tests for the detection of brucellosis in unvaccinated animals; however diagnosis must not be made on the basis of positive intradermal reactions alone. U.K.
(c) Bovine animals, tested with negative result in one of the serological tests defined in this Annex and reacting positively to the BST shall be regarded as infected or suspected to be infected. U.K.
(d) Bovine animals, tested with positive result in one of the serological tests defined in this Annex may be subject to a BST in order to support the interpretation of the serological test results; in particular where in officially brucellosis-free or brucellosis-free bovine herds a cross-reaction with antibodies against other bacteria cannot be excluded. U.K.
3.1.2. The test must be carried out by use of a standardised and defined brucellosis allergen preparation that does not contain smooth lipopolysaccharide (LPS) antigen, as this may provoke non-specific inflammatory reactions or interfere with subsequent serological tests. U.K.
The requirements for the production of brucellin shall comply with Section C1 of Chapter 2.4.3 of the OIE Manual of Diagnostic Tests and Vaccines for Terrestrial Animals, Sixth Edition, 2008.
3.1.3. Test procedure U.K.
3.1.3.1. A volume of 0.1 ml of brucellosis allergen shall be injected intradermally into the caudal fold, the skin of the flank, or the side of the neck. U.K.
3.1.3.2. The test shall be read after 48- to 72-hours. U.K.
3.1.3.3. The skin thickness at the injection site shall be measured with vernier callipers before injection and at re-examination. U.K.
3.1.3.4. Interpretation of results: U.K.
Strong reactions are easily recognised by local swelling and induration.
Skin thickening of 1 to 2 mm shall be considered as positive reaction to the BST.
3.2. Competitive enzyme-linked immunosorbent assay (cELISA) U.K.
3.2.1. Conditions for the use of cELISA U.K.
The cELISA shall not be used for the purpose of certification for intra-Community trade.
Bovine animals, tested with positive result in one of the other serological tests defined in this Annex may be subject to a cELISA in order to support the interpretation of the other serological test results; in particular where in the officially brucellosis-free or brucellosis-free bovine herds a cross-reaction with antibodies against other bacteria cannot be excluded or to eliminate reactions due to residual antibodies produced in response to vaccination with S19.
3.2.2. Test procedure U.K.
The test shall be carried out in accordance with the prescription in Section B(2) of Chapter 2.4.3 of the OIE Manual of Diagnostic Tests and Vaccines for Terrestrial Animals, Sixth Edition, 2008.]
4. NATIONAL REFERENCE LABORATORIES U.K.
4.1. Tasks and responsibilities U.K.
[F6National reference laboratories designated in accordance with Article 6a shall be responsible for:]
the approval of the results of the validation studies demonstrating the reliability of the test method used in the Member State;
determination of the maximum number of samples to be pooled in ELISA kits used;
calibration of the standard secondary reference national standard sera ( ‘ working standards ’ ) against the primary international standard serum referred to in paragraph 2.1;
quality checks of all antigens and ELISA kits batches used in the Member State;
cooperation within the European Union Network of National Reference Laboratories for Brucellosis.]
F7. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .U.K.
[F2ANNEX D U.K.
CHAPTER I U.K. OFFICIALLY ENZOOTIC-BOVINE-LEUKOSIS-FREE HERDS, MEMBER STATES AND REGIONS
A. Officially enzootic-bovine-leukosis-free herd means a herd in which: U.K.
there is no evidence, either clinical or as a result of a laboratory test, of any case of enzootic bovine leukosis in the herd and no such case has been confirmed in the previous two years; and
all animals over 24 months of age have reacted negatively during the preceding 12 months to two tests carried out in accordance with this Annex, at an interval of at least four months; or
it meets the requirements of (i) above and is situated in an officially enzootic-bovine-leukosis-free Member State or region.
B. A herd shall retain officially enzootic-bovine-leukosis-free status provided: U.K.
the condition in A(i) continues to be fulfilled;
any animals introduced into the herd come from an officially enzootic-bovine-leukosis-free herd;
all animals over 24 months of age continue to react negatively to a test carried out in accordance with Chapter II at intervals of three years;
breeding animals introduced into a herd and originating from a third country have been imported in accordance with Directive 72/462/EEC.
C. The officially leukosis-free status of a herd is to be suspended if the conditions detailed in B are not fulfilled, or where as a result of laboratory tests or on clinical grounds one or more bovine animals are suspected of having enzootic bovine leukosis and the suspect animal(s) are immediately slaughtered. U.K.
D. The status is to remain suspended until the following requirements are complied with: U.K.
If a single animal in an officially enzootic-bovine-leukosis-free herd has reacted positively to one of the tests referred to in Chapter II, or where infection is otherwise suspected in one animal in a herd:
the animal which has reacted positively, and, in the case of a cow, any calf it may have produced, must have left the herd for slaughter under the supervision of the veterinary authorities;
all animals in the herd more than 12 months old have reacted negatively to two serological tests (at least 4 months and less than 12 months apart) carried out in accordance with Chapter II three months at least after removal of the positive animal and any possible progeny thereof;
an epidemiological inquiry has been conducted with negative results and the herds linked epidemiologically to the infected herd have been subjected to the measures laid down in (ii).
However, the competent authority may grant a derogation from the obligation to slaughter the calf of an infected cow where it was separated from its mother immediately after calving. In this case, the calf must be made subject to the requirements provided for in 2(iii).
Where more than one animal from an officially enzootic-bovine-leukosis-free herd has reacted positively to one of the tests referred to in Chapter II, or where infection has otherwise been suspected in more than one animal in a herd:
any animals which have reacted positively and, in the case of cows, their calves, must be removed for slaughter under the supervision of the veterinary authorities;
all animals in the herd aged over 12 months must react negatively to two tests carried out in accordance with Chapter II at an interval of at least four months and no more than 12 months;
all other animals in the herd must, after identification, remain on the holding until they are aged over 24 months and have been tested in accordance with Chapter II after reaching that age, except that the competent authority may permit such animals to go directly for slaughter under official supervision;
an epidemiological inquiry has been conducted with negative results and any herd linked epidemiologically to the infected herd has been subjected to the measures laid down in (ii).
However, the competent authority may grant a derogation from the obligation to slaughter the calf of an infected cow where it was separated from its mother immediately after calving. In this case, the calf must be made subject to the requirements provided for in 2(iii).
E. In accordance with the procedure in Article 17 and on the basis of information supplied in accordance with Article 8, a Member State or part of a Member State may be considered officially enzootic-bovine-leukosis-free if: U.K.
all the conditions of paragraph A are fulfilled and at least 99,8 % of the bovine herds are officially enzootic-bovine-leukosis-free;
or
no case of enzootic bovine leukosis has been confirmed in the Member State or the part of the Member State for the past three years, and the presence of tumours suspected of being due to EBL is compulsorily notifiable, with investigations of cause being carried out, and
in the case of a Member State, all animals aged over 24 months in at least 10 % of the herds, selected randomly, have been tested with negative results in accordance with Chapter II in the previous 24 months, or
in the case of a part of a Member State, all animals aged over 24 months have undergone a test provided for in Chapter II with negative results in accordance with Chapter II in the previous 24 months;
or
any other method which demonstrates to a confidence rating of 99 % that less than 0,2 % of herds were infected.
F. A Member State or a region of a Member State is to retain officially enzootic-bovine-leukosis-free status if: U.K.
all animals slaughtered within the territory of that Member State or region are submitted to official post-mortem examinations at which all tumours which could be due to the EBL virus are sent for laboratory examination,
the Member State reports to the Commission all cases of enzootic bovine leukosis that occur in the region,
all animals which react positively to any of the tests provided for in Chapter II are slaughtered and their herds remain subject to restrictions until re-establishment of their status in accordance with Section D, and
all animals more than two years old have been tested, either once in the first five years after the status is granted under Chapter II or during the first five years after the grant of the status under any other procedure demonstrating with a certainty level of 99 % that less than 0,2 % of herds have been infected. However, where no case of enzootic bovine leukosis has been recorded in a Member State or in a region of a Member State in a proportion of one herd out of 10 000 for at least three years, a decision may be taken in accordance with the procedure laid down in Article 17 that routine serological tests may be reduced provided that all bovine animals more than 12 months old in at least 1 % of herds, selected at random each year, have been subjected to a test carried out in accordance with Chapter II.
G. The officially enzootic-bovine-leukosis-free status of a Member State or part of a Member State is to be suspended, in accordance with the procedure in Article 17 if, as a result of investigations carried out in accordance with paragraph F above, there is evidence of a significant change in the situation as regards enzootic bovine leukosis in a Member State or part of a Member State which has been recognised as officially enzootic-bovine-leukosis-free. U.K.
The officially enzootic-bovine-leukosis-free status may be restored in accordance with the procedure in Article 17 when the criteria laid down by the same procedure are fulfilled.]
[F10CHAPTER II U.K. TESTS FOR ENZOOTIC BOVINE LEUKOSIS
Tests for enzootic bovine leukosis shall be carried out by the agar gel immuno-diffusion test (AGID) under the conditions described in Sections A and B or by the enzyme-linked immunosorbent assay (ELISA) under the conditions described in Section C. The agar gel immuno-diffusion test may only be used for the testing of individual samples. If test results are the subject of a duly-substantiated challenge, an additional check shall be carried out by means of the agar gel immuno-diffusion test.
The AGID and ELISA shall be standardised against the E05 serum, which shall be the official EU standard serum, to be supplied by the:
Friedrich-Loeffler-Institut
Federal Research Institute for Animal Health
OIE Reference Laboratory for Enzootic Bovine Leukosis (EBL)
Südufer 10
17493 Greifswald — Insel Riems
Germany.
A. Agar gel immuno-diffusion test for enzootic bovine leukosis U.K.
1. The antigen to be used in the test shall contain bovine leukosis virus glycoprotein. The antigen shall be standardised against the E05 serum. U.K.
2. The State institutes, national reference laboratories or official institutes designated in accordance with Article 6a for coordinating standards and methods of diagnosis of the tests for enzootic bovine leukosis shall be made responsible for calibrating the standard working antigen of the laboratory against the E05 serum. U.K.
3. The standard antigens used in the laboratory shall be submitted at least once a year to the State institutes, national reference laboratories or official institutes designated in accordance with Article 6a, for testing against the E05 serum. Apart from such standardisation, the antigen in use may be calibrated in accordance with the method described in Section B. U.K.
4. The reagents of the tests shall consist of: U.K.
antigen: the antigen shall contain specific glycoprotein of enzootic bovine leukosis virus which has been standardised against the E05 serum;
the test serum;
known positive control serum;
agar gel:
0,8 % agar,
8,5 % NaCl,
0,05 M Tris-buffer pH 7,2,
15 ml of this agar shall be introduced into a petri dish of 85 mm diameter, resulting in a depth of 2,6 mm of agar.
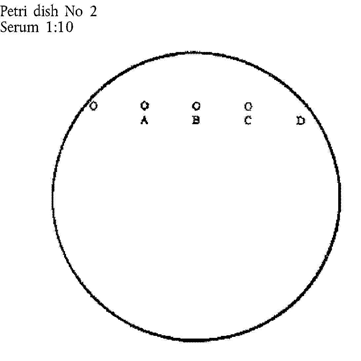
5. A test pattern of seven moisture-free wells shall be cut in the agar to the bottom of the plate; the pattern shall consist of one central well and six wells in a circle around it. U.K.
Diameter of central well: 4 mm
Diameter of peripheral wells: 6 mm
Distance between central and peripheral wells: 3 mm
6. The central well shall be filled with the standard antigen. Peripheral wells 1 and 4 described in B.3 are filled with the known positive serum; wells 2, 3, 5 and 6 with the test sera. The wells shall be filled until the meniscus disappears. U.K.
7. This results in the following quantities being obtained: U.K.
antigen: 32 μl,
control serum: 73 μl,
test serum: 73 μl.
8. Incubation shall be for 72 hours at room temperature (20 to 27 °C) in a closed humid chamber. U.K.
9. The test may be read at 24 and 48 hours but a final result shall not be obtained before 72 hours: U.K.
a test serum is positive if it forms a specific precipitation line with the bovine leukosis virus (BLV) antigen and forms a complete line of identity with the control serum;
a test serum is negative if it does not form a specific precipitation line with the BLV antigen and if it does not bend the line of the control serum;
the reaction cannot be considered conclusive if it:
bends the line of the control serum towards the BLV antigen well without forming a visible precipitin line with the antigen; or
if it cannot be read either as negative or as positive.
In inconclusive reactions the test may be repeated and concentrated serum utilised.
10. Any other well configuration or pattern may be utilised provided that the E05 serum diluted 1:10 in negative serum can be detected as positive. U.K.
B. Method for antigen standardisation U.K.
1. Solutions and materials required: U.K.
40 ml of 1,6 % agarose in 0,05 M Tris/HCl buffer, pH 7,2 with 8,5 % NaCl;
15 ml of a bovine leukosis serum, having antibody only to bovine leukosis virus glycoproteins, diluted 1:10 in 0,05 M Tris/HCl buffer, pH 7,2 with 8,5 % NaCl;
15 ml of a bovine leukosis serum, having antibody only to bovine leukosis virus glycoproteins, diluted 1:5 in 0,05 M Tris/HCl buffer, pH 7,2 with 8,5 % NaCl;
four plastic petri dishes with a diameter of 85 mm;
a punch with a diameter of 4 to 6 mm;
a reference antigen;
the antigen which is to be standardised;
a water bath (56 °C).
2. Procedure: U.K.
Dissolve the agarose (1,6 %) in the Tris/HCl buffer by carefully heating to 100 °C. Place in 56 °C water bath for approximately 1 hour. Also, place the bovine leukosis serum dilutions in a 56 °C water bath.
Now mix 15 ml of the 56 °C agarose solution with the 15 ml bovine leukosis serum (1:10), quickly shake and pour 15 ml into each of two petri dishes. Repeat this procedure with the bovine leukosis serum diluted 1:5.
When the agarose has hardened, holes shall be made in it as follows:
3. Addition of antigen: U.K.
petri dishes 1 and 3:
well A — undiluted reference antigen;
well B — 1:2 diluted reference antigen;
wells C and E — reference antigen;
well D — undiluted test antigen;
petri dishes 2 and 4:
well A — undiluted test antigen;
well B — 1:2 diluted test antigen;
well C — 1:4 diluted test antigen;
well D — 1:8 diluted test antigen.
4. Additional instructions: U.K.
the experiment shall be carried out with two serum dilutions (1:5 and 1:10) in order to achieve optimal precipitation;
if the precipitation diameter is too small with both dilutions, then the serum shall be further diluted;
if the precipitation diameter in both dilutions is too large and faint, then a lower serum shall be chosen;
the final concentration of the agarose shall be 0,8 %; that of the sera 5 and 10 % respectively;
plot the measured diameters in the following coordinate system. The dilution of the antigen to be tested with the same diameter as the reference antigen is the working dilution.
C. Enzyme-linked immunosorbent assay (ELISA) for detecting enzootic bovine leukosis U.K.
1. The material and reagents to be used shall be as follows: U.K.
solid-phase microplates, cuvettes or any other solid phase;
the antigen is fixed to the solid phase with or without the aid of polyclonal or monoclonal catching antibodies. If antigen is coated directly to the solid phase, all test samples giving positive reactions have to be retested against the control antigen. The control antigen should be identical to the antigen except that the BLV antigens are absent. If catching antibodies are coated to the solid phase, the antibodies shall not react to antigens other than BLV antigens;
the biological fluid to be tested;
a corresponding positive and negative control;
conjugate;
a substrate adapted to the enzyme used;
a stopping solution, if necessary;
solutions for the dilution of the test samples for preparations of the reagents and for washing;
a reading system appropriate to the substrate used.
2. Standardisation and sensitivity of test U.K.
The sensitivity of the ELISA shall be of such a level that the E05 serum is scored positive when diluted 10 times (serum samples) or 250 times (milk samples) more than the dilution obtained of individual samples when these are included in pools. In assays where samples (serum and milk) are tested individually, the E05 serum diluted 1 to 10 (in negative serum) or 1 to 250 (in negative milk) shall be scored positive when tested in the same assay dilution as used for the individual test samples. The institutes referred to in point 2 of Section A shall be responsible for checking the quality of the ELISA, and in particular for determining, for each production batch, the number of samples to be pooled on the basis of the count obtained for the E05 serum.
3. Conditions for use of the ELISA for enzootic bovine leukosis U.K.
ELISAs may be used on serum and milk samples.
Where ELISAs are used for certification purposes in accordance with Article 6(2)(c) or for the establishment and maintenance of a herd status in accordance with Annex D(I), pooling of samples of serum or milk shall be carried out in such a way that the samples taken for examination can be undoubtedly related to the individual animals included in the pool. Any confirmatory test shall be carried out on samples taken from individual animals.
Where ELISAs are used on a sample of bulk milk this sample shall be taken from the milk collected from a herd with at least 30 % of dairy cows in milk. Any confirmatory test shall be carried out on samples of serum or milk taken from individual animals.]
Textual Amendments
ANNEX E (I) U.K.
(a) Bovine diseases U.K.
Foot-and-mouth disease
Rabies
Tuberculosis
Brucellosis
Contagious bovine pleuropneumonia
Enzootic bovine leukosis
Anthrax
(b) Swine diseases U.K.
Rabies
Brucellosis
Classical swine fever
African swine fever
Foot-and-mouth disease
Swine vesicular disease
Anthrax
ANNEX E (II) U.K.
Aujeszky's disease
Infectious bovine rhinotracheitis
Brucella suis infection
Transmissible gastro-enteritis
[F2ANNEX F U.K.
Model 1 U.K.
Model 2 U.K.
Textual Amendments
F1 Substituted by Council Directive 97/12/EC of 17 March 1997 amending and updating Directive 64/432/EEC on health problems affecting intra-Community trade in bovine animals and swine.
Options/Cymorth
Print Options
PrintThe Whole Directive
PrintThe Annexes only
You have chosen to open the Whole Directive
The Whole Directive you have selected contains over 200 provisions and might take some time to download. You may also experience some issues with your browser, such as an alert box that a script is taking a long time to run.
Would you like to continue?
Mae deddfwriaeth ar gael mewn fersiynau gwahanol:
Y Diweddaraf sydd Ar Gael (diwygiedig):Y fersiwn ddiweddaraf sydd ar gael o’r ddeddfwriaeth yn cynnwys newidiadau a wnaed gan ddeddfwriaeth ddilynol ac wedi eu gweithredu gan ein tîm golygyddol. Gellir gweld y newidiadau nad ydym wedi eu gweithredu i’r testun eto yn yr ardal ‘Newidiadau i Ddeddfwriaeth’.
Gwreiddiol (Fel y’i mabwysiadwyd gan yr UE): Mae'r wreiddiol version of the legislation as it stood when it was first adopted in the EU. No changes have been applied to the text.
Pwynt Penodol mewn Amser: This becomes available after navigating to view revised legislation as it stood at a certain point in time via Advanced Features > Show Timeline of Changes or via a point in time advanced search.
Gweler y wybodaeth ychwanegol ochr yn ochr â’r cynnwys
Rhychwant ddaearyddol: Indicates the geographical area that this provision applies to. For further information see ‘Frequently Asked Questions’.
Dangos Llinell Amser Newidiadau: See how this legislation has or could change over time. Turning this feature on will show extra navigation options to go to these specific points in time. Return to the latest available version by using the controls above in the What Version box.
Rhagor o Adnoddau
Gallwch wneud defnydd o ddogfennau atodol hanfodol a gwybodaeth ar gyfer yr eitem ddeddfwriaeth o’r tab hwn. Yn ddibynnol ar yr eitem ddeddfwriaeth sydd i’w gweld, gallai hyn gynnwys:
- y PDF print gwreiddiol y fel adopted version that was used for the EU Official Journal
- rhestr o newidiadau a wnaed gan a/neu yn effeithio ar yr eitem hon o ddeddfwriaeth
- pob fformat o’r holl ddogfennau cysylltiedig
- slipiau cywiro
- dolenni i ddeddfwriaeth gysylltiedig ac adnoddau gwybodaeth eraill
Llinell Amser Newidiadau
Mae’r llinell amser yma yn dangos y fersiynau gwahanol a gymerwyd o EUR-Lex yn ogystal ag unrhyw fersiynau dilynol a grëwyd ar ôl y diwrnod ymadael o ganlyniad i newidiadau a wnaed gan ddeddfwriaeth y Deyrnas Unedig.
Cymerir dyddiadau fersiynau’r UE o ddyddiadau’r dogfennau ar EUR-Lex ac efallai na fyddant yn cyfateb â’r adeg pan ddaeth y newidiadau i rym ar gyfer y ddogfen.
Ar gyfer unrhyw fersiynau a grëwyd ar ôl y diwrnod ymadael o ganlyniad i newidiadau a wnaed gan ddeddfwriaeth y Deyrnas Unedig, bydd y dyddiad yn cyd-fynd â’r dyddiad cynharaf y daeth y newid (e.e. ychwanegiad, diddymiad neu gyfnewidiad) a weithredwyd i rym. Am ragor o wybodaeth gweler ein canllaw i ddeddfwriaeth ddiwygiedig ar Ddeall Deddfwriaeth.
Rhagor o Adnoddau
Defnyddiwch y ddewislen hon i agor dogfennau hanfodol sy’n cyd-fynd â’r ddeddfwriaeth a gwybodaeth am yr eitem hon o ddeddfwriaeth. Gan ddibynnu ar yr eitem o ddeddfwriaeth sy’n cael ei gweld gall hyn gynnwys:
- y PDF print gwreiddiol y fel adopted fersiwn a ddefnyddiwyd am y copi print
- slipiau cywiro
liciwch ‘Gweld Mwy’ neu ddewis ‘Rhagor o Adnoddau’ am wybodaeth ychwanegol gan gynnwys
- rhestr o newidiadau a wnaed gan a/neu yn effeithio ar yr eitem hon o ddeddfwriaeth
- manylion rhoi grym a newid cyffredinol
- pob fformat o’r holl ddogfennau cysylltiedig
- dolenni i ddeddfwriaeth gysylltiedig ac adnoddau gwybodaeth eraill